In an era of data-rich healthcare, predictive analytics is rapidly becoming an essential tool for hospitals aiming to improve patient outcomes and optimize care delivery. According to a recent Deloitte report, 60% of healthcare organizations are already using some form of predictive modeling — yet many struggle with implementation, accuracy, or workflow integration.
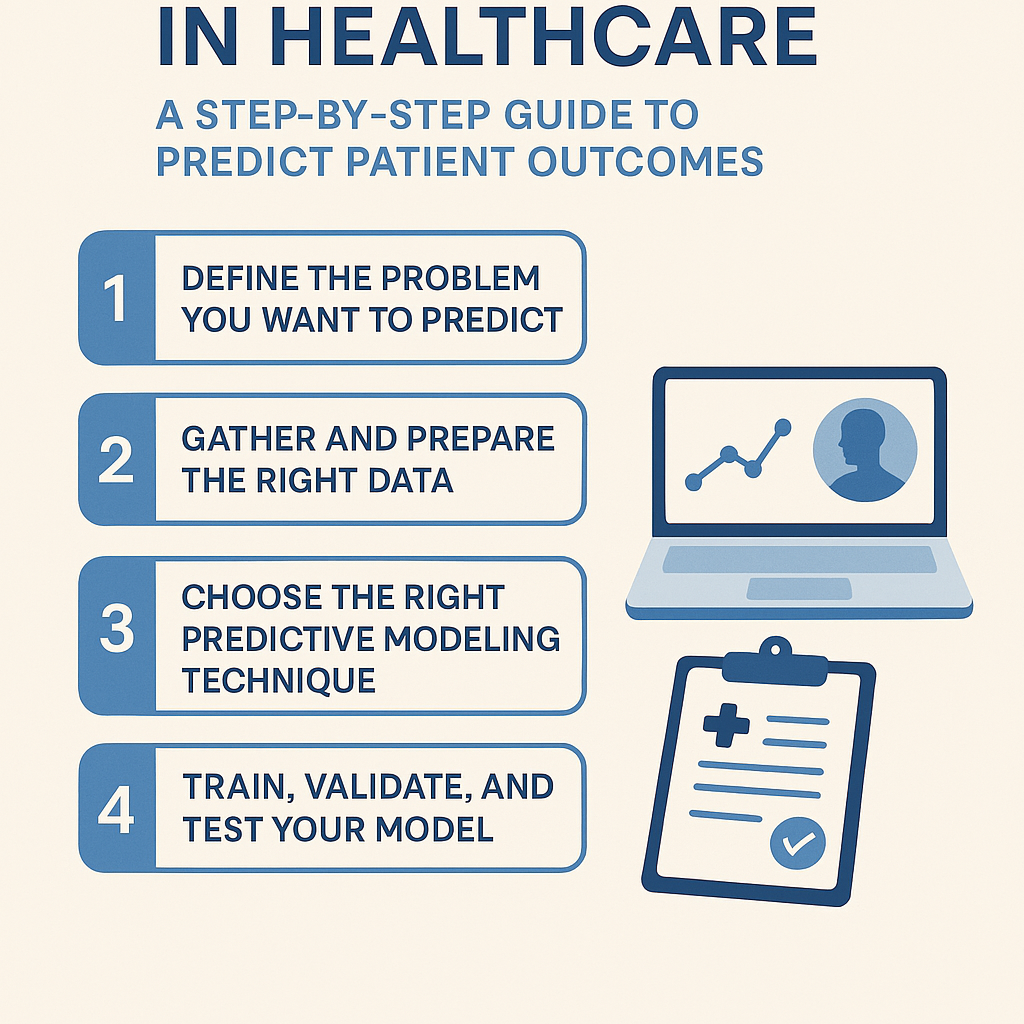
This guide provides a step-by-step walkthrough for clinical data analysts, public health data scientists, and healthcare decision-makers looking to apply predictive analytics in healthcare. You'll learn how to prepare your data, choose the right models, and evaluate predictions, all with the goal of improving how hospitals predict patient outcomes.
Step 1: Define the Problem You Want to Predict
Before building a model, clearly define the health outcome you're trying to predict. This might include:
- Hospital readmissions within 30 days
- Risk of ICU transfer
- Likelihood of medication non-adherence
- Disease progression timelines (e.g., diabetes or CHF)
Be specific — "improving patient health" is not a predictive question. Instead, frame your target as a binary or continuous variable: Will this patient be readmitted within 30 days? What is the risk score of sepsis in the next 12 hours?
Step 2: Gather and Prepare the Right Data
Effective predictive modeling hinges on high-quality, relevant data. For healthcare, this often means:
- EHR data (diagnoses, vitals, medications, labs)
- Claims data
- Patient-reported outcomes
- Social determinants of health (SDOH)
Clean and preprocess your data by:
- Handling missing values appropriately (imputation or removal)
- Encoding categorical variables (one-hot, label encoding)
- Normalizing or scaling features
- Ensuring temporal integrity — training on data before outcomes occurred
📌 Tip: Bias in the data (e.g., under-diagnosis in marginalized populations) can lead to biased predictions. Always audit your features for representativeness.
Step 3: Choose the Right Predictive Modeling Technique
The model you choose depends on your outcome type and the complexity of the data:
| Outcome Type | Example | Recommended Models |
|---|---|---|
| Binary | Readmitted: Yes/No | Logistic Regression, Random Forest |
| Multiclass | Diagnosis Type | Gradient Boosted Trees, XGBoost |
| Continuous | Length of Stay (LOS) | Linear Regression, SVR |
| Time-to-Event | Mortality risk in 6 mo. | Survival Analysis, Cox Regression |
More advanced use cases might leverage deep learning (e.g., LSTMs for time series vitals) or ensemble models for better accuracy.
Step 4: Train, Validate, and Test Your Model
Split your dataset into training, validation, and testing sets — typically in a 60/20/20 ratio. Avoid data leakage by ensuring that patient records don't appear in more than one subset.
Evaluate your model using metrics relevant to healthcare decision-making:
- AUROC (Area Under ROC Curve) – great for binary classification
- Precision/Recall – especially important for high-risk predictions
- F1 Score – balances precision and recall
- Calibration plots – show how predicted probabilities match actual outcomes
Remember: A model with high accuracy might still perform poorly in clinical practice if it lacks interpretability or generalizability.
Step 5: Interpret and Operationalize the Predictions
Predictions must be explainable, especially in healthcare settings where clinicians and administrators need to trust the output. Techniques like SHAP values or LIME can help make model outputs more transparent.
To operationalize predictions:
- Integrate them into clinical workflows (e.g., EHR alerts)
- Develop decision pathways triggered by specific risk thresholds
- Monitor model performance over time for drift or degradation
How Statsource Can Help
Tools like Statsource streamline the process of running machine learning predictions on health outcomes. From data ingestion and cleaning to model selection and interpretability, Statsource helps healthcare analysts implement predictive analytics without starting from scratch.
Whether you're testing logistic regression models for readmission or exploring time-series predictions for ICU alerts, Statsource enables rapid iteration, statistical rigor, and reproducibility — all tailored for the nuances of healthcare data.
Final Thoughts
Predictive analytics in healthcare is not just a technical exercise — it's a strategic opportunity to transform patient care. By following a structured approach, clinical data teams can predict patient outcomes with increasing accuracy and clinical relevance.
With the right data, models, and tools, healthcare organizations can move from reactive care to proactive intervention.
💡 Ready to apply predictive analytics? Try using Statsource to explore predictive modeling on your healthcare data and improve patient outcomes.
Explore more how-tos and healthcare data science guides at healthstats.info.